EMS Clinical Introduction
Welcome to CCFES' EMS Clinical

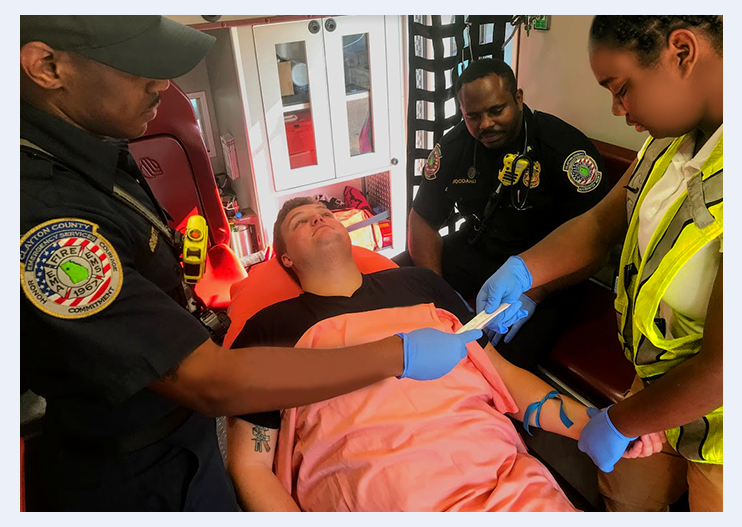
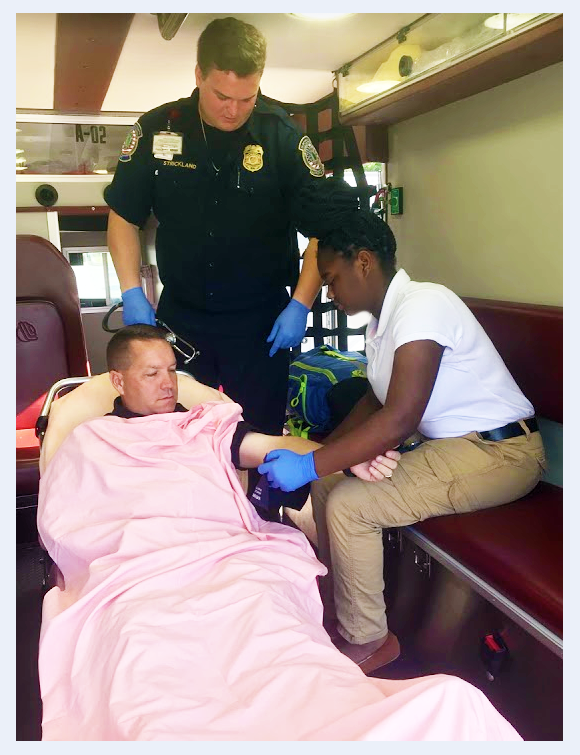
Clinical education is an important aspect of any professional health care program. It provides students with an opportunity to:
- Integrate theory and practical skills in the treatment of actual patients.
- Visualize signs such as pale skin,
diaphoresis, changes in papillary response and other symptoms
important for patient assessment and management.
- Perform skills on live patients in the clinical setting.
- Observe expert clinical practice, including
communications with patients, peers, and the EMS 911 system.
- Complete assessments, observe decision-making, and set priorities
- Observe professional treatment plans by EMS and/or allied health care
professionals.
Clinical Prerequisites
Students are required to show proof of the following before beginning of any clinical rotations:
· Current negative PPD test (or neg. Chest X-ray)
· Proof of MMR Vaccination
· Proof of first injection of Hepatitis‑B series
· Signed Health Form
· Malpractice Insurance
· Successful completion of a 10-Panel Drug Screen (including Opiates)
· Successful completion of NCIC Criminal Background Check
· Complete Uniform – Shirt, Pants, Shoes, Belt, Watch with Second Hand or Seconds Digital Readout, CCFES ID Badge and/or Clinical Site ID Badge
· Current Registration in Clinical Portion of EMT, AEMT or paramedic program at Clayton County Fire and Emergency Services
CLINICAL SCHEDULE

CCFES has selected clinical facilities within Clayton County based on their willingness to allow our students access, the high level of quality experiences, and the variety and volume of patients served.
Currently, students in both AEMT and paramedic class are able to access Southern Regional Medical Center for clinical rotations.
The clinical schedule is submitted to the respective clinical site for approval one month before the actual start date. Students may not begin until the official schedule is approved by the clinical site and the instructor has given their permission.
Clinical dates will depend on availability at given facility and CCFES' operations schedule. Some flexibility will be permitted whenever possible. Once closed, the schedule is FINAL and students are committed to their dates; however, swaps can be made on an individual basis at the discretion of the EMS clinical coordinator and/or the class lead instructor. Both students involved must agree, be willing to swap, and complete the appropriate paperwork.
All clinical shifts will be performed in a minimum of 6-hour shifts.
Clinical Agency Policies
A contractual agreement between the department and the participating facility means that all students are expected to abide by their rules and regulations. Failing to or refusing to abide by these policies will mean that department personnel or students will not be permitted to care for patients and may be dismissed for noncompliance.
 Students who are dismissed from clinical experiences may jeopardize their ability to satisfactorily complete the course requirements, and may be dropped from the program.
Students who are dismissed from clinical experiences may jeopardize their ability to satisfactorily complete the course requirements, and may be dropped from the program.Problems at Clinical Facilities
Any problems arising during clinicals including personal conflicts with preceptors or supervisors, should be handled with the utmost professionalism. Remember that students are guests at the clinical facilities and should present non-confrontational attitudes whenever possible. The student should notify the clinical coordinator or lead instructor as soon as possible concerning any problems encountered during a clinical rotation.
EMS Clinical Preceptors
The clinical component of the EMS course exposes students to real world experiences. Our clinical preceptors are chosen and certified to mentor, observe, and give constructive feedback to the new EMS student during their scheduled clinical. They serve as the student’s primary source of practical emergency care knowledge on an emergency scene and in the clinical setting. Their objectives are aligned to reinforce the student’s knowledge and skills before completing a final performance evaluation.
The student must be under direct supervision during this phase of training. Physicians, registered nurses, and EMS preceptors in each of the clinical areas will provide supervision and guidance to keep students and patients safe during the clinical.
The student's performance will be closely observed and evaluated by the clinical preceptor and/or the EMS ride along clinical instructor to determine whether the student demonstrates appropriate application of knowledge and skills acquired during the didactic and psychomotor portion of their education.
Accurate documentation of clinical experiences is essential for course completion.
Clinical Documentation
A Student Performance Evaluation must be completed for each clinical shift and be signed by a state-certified EMS preceptor. Records without appropriate signatures will not count toward clinical experience requirements.
- The student must document the skills they completed during each clinical shift.
- During EMS/ambulance rotations, a minimum of 10 PCRs for EMT students, 20 PCRs for AEMT students and 20 PCRs for paramedic students must be completed. These reports will include: MOI/NOI, patient gender and age (no personal information), past medical history, medications, and narrative (including vitals, treatments, and procedures). CPR or call numbers are to be written on the evaluation form before turning it in for credit.
NOTE: A complete clinical notebook must be submitted to the lead instructor or clinical coordinator by the required deadline(s). Failure to submit documentation may result in a reduction of the clinical grade or possible dismissal from the program.
Only experiences/skills signed off by an instructor or preceptor will count toward program requirements. A list of CCFES EMS Preceptors can be found on the computer located at each station under: Station Forms/Training/EMS Preceptors.
FALSIFICATION OF ANY RECORDS PERTAINING TO CLINICALS CONSTITUTES CHEATING AND IS GROUNDS FOR IMMEDIATE DISMISSAL FROM THE PROGRAM.
STUDENT CONDUCT & EXPECTATIONS
Because their conduct reflects upon the individual, clinical site, and Clayton County Fire & Emergency Services, the EMS student must conduct himself/herself in a professional, mature manner at all times.
Students should give their full attention and respect to the preceptors. Any questions that arise during the clinical setting that are not answered in a way that enhances learning or understanding should be brought back to the classroom and to the instructional faculty for further explanation.
Any student may be dismissed from the program for unacceptable behavior during clinical performance. EMS students will adhere to all policies and any additional rules or procedures explained by the Training Academy staff. Failure to comply will result in disciplinary action and possible dismissal from the program.
It is the student’s responsibility to be aware of all clinical requirements, program requirements, and department requirements for completion as stated in the syllabus. Both the clinical preceptor and clinical site have the option of sending a student home if they feel he or she is in violation of appropriate conduct.
The student will complete a set of skills during the clinical "ride along to prepare them to function on real emergency calls. Preceptors will evaluate each student on their current knowledge and ability to perform the medical skills required by the State Office of EMS and Clayton County Fire & Emergency Services.
Medications
Absolutely NO alcohol, drugs, or medications will be ingested 24 hours prior to or during a clinical assignment. The exceptions are prescription medications that are required to maintain health and/or manage chronic medical conditions, Advil or equivalent, and Tylenol or equivalent. Prescription narcotics or other medication (including over-the-counter) that have the potential to impair your judgment and/or your ability to function should not be taken 24 hours prior to clinical or during your clinical shift. Violation of the drug and alcohol provision will result in immediate expulsion from the clinical site and permanent dismissal from the EMS program. Any questions should be brought to the attention of the Lead Instructor.
Exposures
Any improper/illegal conduct or intentional unsafe act at the clinical site will result in automatic, permanent expulsion from the site and EMS programs. If the student becomes injured, receives an accidental needle stick, or is exposed to any infectious disease during the clinical experiences they MUST IMMEDIATELY CONTACT THE LEAD INSTRUCTOR OR CLINICAL COORDINATOR and complete all department/program required documentation.
CLINICAL UNIFORM STANDARDS
When in uniform, students represent the EMS profession and their sponsoring EMS Program. They also represent the affiliated agency where they are practicing. It is critical that all students project a professional image to everyone they encounter. All students must arrive on time and be neatly groomed and professionally dressed as required by industry and work standards.
Shorts, jeans, t-shirts,
sandals, tennis shoes and scrubs (see exception below) are not allowed. If a student’s uniform becomes soiled during the
clinical experience, the student is permitted to wear surgical scrubs, if
available and permission is obtained from the preceptor.
THERE ARE NO EXCEPTIONS FOR NOT REPORTING IN THE APPROVED UNIFORM.
The clinical site has the option to send any student home if he/she is inappropriately dressed, disheveled, TARDY or for violation of any clinical facilities’ policies. Being sent home for a uniform issue will only be allowed once. Repeated offenders will not be allowed to complete the clinical portion and will be dismissed from the program.
CLINICAL UNIFORM REQUIREMENTS
- Student ID – Clayton County Fire & Emergency Services EMS Student ID will be distributed by the clinical coordinator before your first scheduled clinical shift and be worn at all times. It may also be required to wear an ID badge of the clinical site they are attending. (Southern Regional, Grady, etc.). Loss of ID badge will result in a $20 fee payable upon issuance of a new ID badge.
- Shoes - Solid black work boots/half boots must be
worn. Shoes should be able to be polished, and WILL be polished prior to arriving at a clinical site. No
clogs, canvas, or open-toed shoes may be worn. For safety reasons steel
toes are preferred.
- Shirt – A red golf shirt with the student ID badge attached to the shirt with the words “EMS Student” printed on the ID). A windbreaker or heavier winter jacket or raincoat may be worn over the golf shirt in inclement weather. Jackets/windbreakers should be a solid neutral color and not bear ANY markings, patches, or other type of logo(s).
- Pants – Standard Navy Blue BDU (unbloused) are to be worn to each clinical site. Pants should be in good condition, clean and pressed prior to arrival at the clinical site. Jeans WILL NOT be worn to clinical sites.
- Hair – Hair will be neatly kept, and must be pulled back in such a manner that it does not fall forward. Facial hair will be limited to a neatly trimmed mustache that does not extend past the border of the lips. Beards will not be permitted due to clinical contracts and infection control practices.
- Nails – Nails must be clean and neatly trimmed flush with the end of the finger. Acrylic nails must be removed. This standard is required to meet clinical contract requirements and infection control practices.
- Jewelry – Only wedding rings, watches, or conservative jewelry having religious meaning may be worn. Earrings or any other visible body piercing are not permitted.
- Tattoos - All visible tattoos must be covered. Small tattoos may be covered with a bandage. Larger tattoos must be covered up with a matching long sleeve undershirt.
- Hygiene - Proper body hygiene is required. Close contact with patients and fellow professionals requires the utmost attention to personal hygiene. Perfumes and colognes shall be avoided.
NOTE: EMPLOYED MEMBERS OF THE CLAYTON COUNTY FIRE & EMERGENCY SERVICES OR ANOTHER STATE OF GEORGIA CERTIFIED FIRE DEPARTMENT ARE ALLOWED TO WEAR THEIR DEPARTMENT UNIFORM IN ITS ENTIRETY INSTEAD THE UNIFORM SHOES/SHIRT/PANTS REQUIREMENTS ABOVE.
*NOTE: All clinical sites reserve the right to deny access to their facilities to any student that willfully and knowingly violates the clinical facilities policies and procedures, EMS program policies and procedures, violates any criminal or civil law, reports to duty impaired by alcohol, medication, or illegal drugs, or is currently ill with any infectious disease that may place their clients or staff at risk of exposure to a contagion. Denial of access to any clinical facility for the above reasons may result in such consequences as unsuccessful completion of the EMS Program, immediate and permanent expulsion from the EMS Program and/or the inability to sit for the National Registry certification exam.
For students with a permanent, chronic illness i.e.: Hepatitis B or C, etc; who have no possible chance of recovery, access to clinical sites may be prohibited permanently by the clinical facility and may lead to the inability of the student to successfully complete the EMT Program requirements.
NOTIFICATION PROCEDURE
Students may only participate in
clinical experiences that have been scheduled by the lead instructor or clinical
coordinator. Whenever possible, students will be assigned a variety of shifts
to meet individual scheduling requirements. All students will follow the
procedure outlined below.
- If you are going
to be absent from a clinical, you must notify the clinical coordinator a
minimum of 15 minutes before the start time of the scheduled clinical shift.
Failure to follow this notification procedure will result in an unexcused
absence and will reduce the clinical grade by 25 points per occurrence.
- If you are going
to be late, you must notify the clinical coordinator as outlined above.
More than 10 minutes late to the clinical site OR from a scheduled lunch/dinner/break is considered a missed
day or an absence; the student may be sent home. Each tardy less than 10
minutes will result in a 5-point reduction of the clinical grade per
occurrence.
- All missed
clinical days regardless of the reason must be made up before the end of
the quarter in which they occurred. Failure to make up clinical time will be considered an incomplete and a “F” will be
recorded as the final grade.
- Failure to abide
by the dress code (neat and professional appearance, no excessive jewelry,
hair neat, etc.) will reduce the clinical grade by 10 points per
occurrence and the student may be sent home.
- Failure to turn in
any clinical assignment on time will reduce the clinical grade by
10 points each day until submitted.
- Failure to be
knowledgeable when administering medications or failure to administer
medications correctly/safely will reduce the clinical grade by 25 points. (If you are unsure of a medication or
how to administer a medication, DO NOT give it to the patient. ASK for help
from your preceptor, instructor, or clinical coordinator.)
- Failure to
demonstrate the appropriate behavior as stated in the EMT Code of Ethics
(see Code of Ethics) and as expected of a medical professional will
reduce the clinical grade by 25 points.
- Failure to follow
clinical preceptor instructions will reduce the clinical grade by
10 points.
- Failure to be
knowledgeable of assigned patient’s condition will reduce the clinical
grade by 10 points.
- Failure to safely conduct oneself including failing to use appropriate Body Substance
Isolation, Personal Protective Equipment, or other infection control
procedures will reduce the grade by 10 points.
Notification Procedure:
EXCUSED ABSENCES/TARDIES: Any
student that is either late or unable to attend a scheduled shift must notify the clinical coordinator a minimum of 15 minutes before the scheduled start time.
Instructor/Clinical Coordinator contact information can be found in the Clinical Contact Folder .
These numbers should be saved in your mobile phone for easy access. If unable to immediately speak with an instructor/clinical coordinator, students must leave a voicemail and continue to try to reach an instructor. If you are absent (excused) for two clinical shifts during the entire clinical rotation, you may be withdrawn from clinical and will be unable to complete the program.
UNEXCUSED ABSENCES/TARDIES: Students with UNEXCUSED absences from
clinical (failure to notify the clinical coordinator) may be placed on
probation (first time) or dismissed from the program (second time). The clinical coordinator will maintain a record
of each student’s clinical attendance.
AT NO TIME ARE STUDENTS ALLOWED TO REARRANGE/RESCHEDULE
THEIR OWN CLINICAL SHIFTS. ANY CLINICAL SHIFT NOT ARRANGED AND APPROVED BY THE LEAD
INSTRUCTOR OR CLINICAL COORDINATOR WILL NOT COUNT TOWARD THE STUDENT'S CLINICAL
REQUIREMENTS. THERE ARE NO EXCEPTIONS TO THIS REQUIREMENT.
ATTENDANCE
All students must report to their clinical preceptor no less than 15
minutes before the start of their shift.
Attendance at a scheduled clinical shift is a requirement. Potential
excused absences are at the discretion of the clinical coordinator.
It is required that each EMS student document all hours worked
on the Clinical Time Sheet.
The student must remain in the assigned area for the entire shift
except for approved breaks. Students may leave their assigned area for one 45-minute
lunch/dinner break. One 15-minute break for each four hour period worked may be
taken. Breaks and/or meals may not be taken at the end of the shift. The
student must request permission from the preceptor before leaving for break or
meals.
TARDINESS
Tardiness is not tolerated. In the
event of tardiness, the student must notify the clinical coordinator (at the
number listed on page 2 of this manual) a minimum of 15 minutes prior to the beginning
of the scheduled time to inform them of the anticipated time of arrival. It is the instruction/clinical coordinator's discretion whether to allow the student
to continue to the site or to receive an unexcused absence. Students must
schedule potential make-up hours for tardiness or leaving early.
A MAXIMUM OF 2 TARDIES WILL BE ALLOWED DURING THE ENTIRE CLINICAL
ROTATION. THREE OR MORE TARDIES MAY RESULT IN DISCIPLINARY ACTIONS INCLUDING
DISMISSAL FROM THE EMS PROGRAM.
ILLNESS
Students who are ill are expected to seek appropriate care and must contact the clinical coordinator no less than at least 15
minutes before the start of their clinical shift to inform them of their
illness. If the student becomes
ill during a rotation, the clinical coordinator must be contacted
immediately. It is the student’s responsibility to contact the clinical
coordinator and make arrangements for possible return to the clinical rotation
and to reschedule the missed hours. The Training Academy may request written
medical approval before allowing the student to return to clinical facilities.
INJURY/EXPOSURE
AND MEDICAL LIABILITY
Safety is of the utmost importance to this program and the student must take their role seriously. If the student is injured or exposed to an infectious disease during a clinical, they must comply with all hospital and program policies.
The student must notify the clinical
coordinator AND their preceptor of the injury or exposure immediately. The student will be advised and counseled as to the appropriate action(s) to
take. Students are required to have medical liability insurance coverage and are financially responsible for any treatment and/or hospitalization required due to injuries
sustained while on a clinical rotation. Failure to comply with this policy may
result in immediate dismissal from the program. In addition, all students must
complete all department/program required documentation.
SCOPE OF PRACTICE
In the clinical setting, the EMS student can perform any activity identified in the scope of practice defined by the Georgia Department of Community Health, Georgia Office of EMS & Trauma. The current Scope of Practice is found in the Clinical Resources folder.
STUDENTS WHO PRACTICE OUTSIDE THEIR SCOPE OF PRACTICE DURING NON PROGRAM RELATED EXPERIENCES ARE IN VIOLATION OF THEIR EXISTING LICENSURE. THEY MAY BE DISCIPLINED OR DROPPED FROM THE EMS PROGRAM.
EMT CODE OF ETHICS
Professional status as an Emergency Medical Technician and Emergency Medical Technician-EMT is maintained and enriched by the willingness of the individual practitioner to accept and fulfill obligations to society, other medical professionals, and the profession of Emergency Medical Technician. As an Emergency Medical Technician, I solemnly pledge myself to the following code of professional ethics:A fundamental responsibility of the Emergency Medical Technician is to conserve life, to alleviate suffering, to promote health, to do no harm, and to encourage the quality and equal availability of emergency medical care.
The Emergency Medical Technician provides services based on human need, with respect for human dignity, unrestricted by consideration of nationality, race creed, color, or status.
The Emergency Medical Technician does not use professional knowledge and skills in any enterprise detrimental to the public well being.
The Emergency Medical Technician respects and holds in confidence all information of a confidential nature obtained in the course of professional work unless required by law to divulge such information.
The Emergency Medical Technician, as a citizen, understands and upholds the law and performs the duties of citizenship; as a professional, the Emergency Medical Technician has the never-ending responsibility to work with concerned citizens and other health care professionals in promoting a high standard of emergency medical care to all people.
The Emergency Medical Technician shall maintain professional competence and demonstrate concern for the competence of other members of the Emergency Medical Services health care team.
An Emergency Medical Technician assumes responsibility in defining and upholding standards of professional practice and education.
The Emergency Medical Technician assumes responsibility for individual professional actions and judgment, both in dependent and independent emergency functions, and knows and upholds the laws which affect the practice of the Emergency Medical Technician.
An Emergency Medical Technician has the responsibility to be aware of and participate in matters of legislation affecting the Emergency Medical Service System.
The Emergency Medical Technician, or groups of Emergency Medical Technicians, who advertise professional service, do so in conformity with the dignity of the profession.
The Emergency Medical Technician has an obligation to protect the public by not delegating to a person less qualified, any service which requires the professional competence of an Emergency Medical Technician
The Emergency Medical Technician will work harmoniously with and sustain confidence in Emergency Medical Technician associates, the nurses, the physicians, and other members of the Emergency Medical Services health care team.
The Emergency Medical Technician refuses to participate in unethical procedures, and assumes the responsibility to expose incompetence or unethical conduct of others to the appropriate authority in a proper and professional manner.
(adopted by the National Association of EMT's)
Written by: Charles Gillespie M.D. Adopted by: The National Association of Emergency Medical Technicians, 1978.